Senior National Hospital Insurance Fund (NHIF) officials are on the spot for turning the fund into an outfit benefitting a select few for specialised treatment abroad at the expense of millions of other beneficiaries.
The accusations came as MPs grilled fund chief executive Nicodemus Odongo, who appeared before the National Assembly’s Health committee on Wednesday.
Consequently, the committee members demanded that NHIF table a list of all individuals, who have been financed to seek treatment abroad since the beginning of 2018.
The members claimed the fund has been deducting money from poor Kenyans to finance healthcare for the rich.
“NHIF is using poor people’s money to fund other people’s healthcare outside Kenya. Let this committee know whether there are hospitals that have not been paid their claims,” said Ugenya MP David Ochieng.
Select beneficiaries
At the same time, Ochieng and his counterparts Eseli Simiyu (Tongaren) and Thuku Kwenya (Kinangop) expressed concern that close to half of the NHIF budget was being used to settle claims from private hospitals at the expense of government and mission hospitals where a majority of poor Kenyans seek treatment.
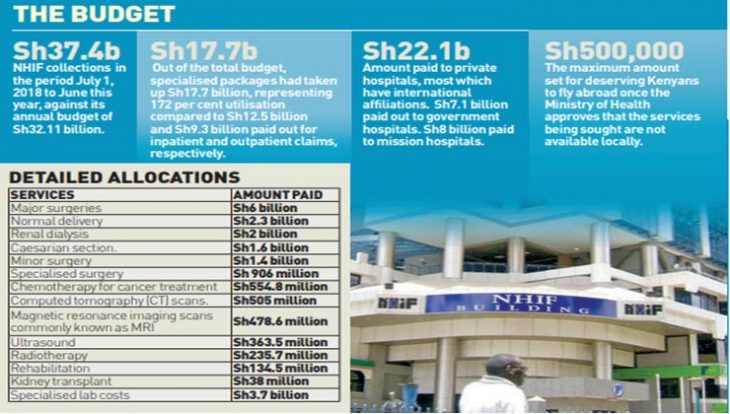
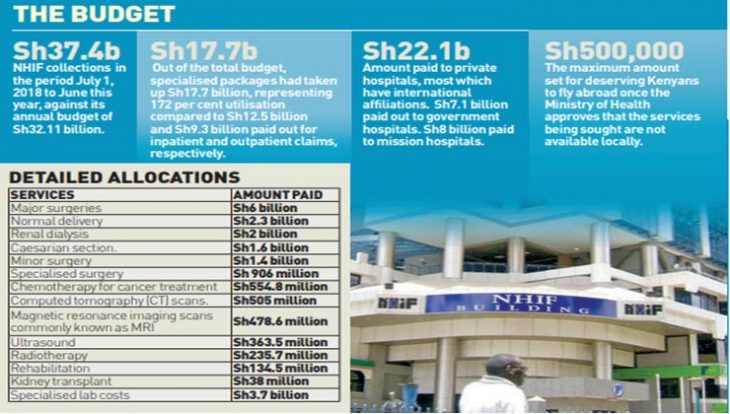
The lawmakers were reacting to documents tabled yesterday by Odongo before the committee that showed that out of Sh37.4 billion in benefits between July 1, 2018 to June this year, private hospitals, most which have international affiliations, had taken the lion’s share—Sh22.1 billion compared to Sh7.1 billion and Sh8 billion paid out to government and mission hospitals, respectively.
Thuku said private hospitals were taking the highest share of the funding “because the fund was paying the rich to seek treatment abroad at the expense of other Kenyans”.
Simiyu sought to know the criteria for selecting those who have so far travelled abroad for specialised treatment.
“How are you selecting those people who are going abroad and who have been covered by NHIF?” he asked.
“It is evident that the poor are financing the rich through your institution,” he added.
Responding to the MPs’ concerns, Odongo admitted that there could be possible loopholes in how the fund offers its specialised packages, but added that the national insurer has pre-authorisation forms that are duly signed by the doctors to ensure the claims are not abused.
He added that in cases where treatment is not locally available, the Health ministry approves such services abroad.
The package is currently capped at Sh500,000.
“The lack of age limits for members, and access to overseas treatment for members of some negotiated schemes pose challenges of financial risks that have seen utilisation steadily go up,” said Odongo
The NHIF report showed that out of the total budget, specialised packages had taken up Sh17.7 billion, representing 172 per cent utilisation compared to Sh12.5 billion and Sh9.3 billion paid out for inpatient and outpatient claims respectively.
Documented expenditure
“Of the money set aside for specialised treatment, the biggest share was taken by major surgeries at Sh6 billion, normal delivery Sh2.3 billion, renal dialysis Sh2 billion, and Caesarian section Sh1.6 billion.
Minor surgery consumed Sh1.4 billion, and specialised surgery Sh906 million,” read the report.
Another Sh554.8 million went into chemotherapy for cancer treatment while Sh505 million catered for computed tomography (CT) scans.
Magnetic resonance imaging scans commonly known as MRI took up Sh478.6 million, ultrasound Sh363.5 million, radiotherapy Sh235.7 million, rehabilitation Sh134.5 million, kidney transplant Sh38 million, and specialised lab costs Sh3.7 billion.